Claims Administration
The length of time it has taken to process the claims is within one to two weeks subjected to submit correct support documents by insure.
The supporting documents are as follow:
- In-Patient’s document requirements:
- Original hospital invoice in their pad including the logo and stamp of hospital. The total treatment expenses shall be supported by a breakdown (i.e. operation expenses, doctor fees, administration fee and etc).
- All medical records (discharge, medical report, receipts, bills and prescriptions and arrange them in chronological order.
- Discharge report.
- Fill out the claim form of IHA and sign it.
- Understand all details in the policy documents.
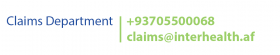
- Submit the claim request by email, whatsapp, viber and other means of communication to IHA, Contact details provided behind the insurance card of employees.
- Out-Patient’s document requirements
- Original invoice for paid visit fee (amount paid) including the full details of patient (name, date) signed and stamp by doctor.
- Original doctor’s medical report including the services performed, stamp and singed by doctor.
- Fill out the claim form of IHA and sign it.
- Submit the claim request by email, whatsapp, viber and other means of communication to IHA, contact details provided behind the insurance card of employees.
- Laboratory (outpatient)’s document requirement:
- Original laboratory invoice in their pad including the full details of patient, signed and stamp.
- Original doctor’s prescription with all required tests, if any.
- Fill out the claim form of IHA and sign it.
- Submit the claim request by email, whatsapp, viber and other means of communication to IHA, contact details provided behind the insurance card of employees.
- Pharmacy (outpatient)’s documents requirement:
- Original pharmacy invoice in their Letter Head including the full details of insured employee, signed and stamp.
- Original doctor’s prescription with all required medications, if any.
- Fill out the claim form of IHA and sign it.
- Submit the claim request by email, whatsapp, viber and other means of communication to IHA, contact details provided behind the insurance card of employees.
Refunding Process:
Reimbursement facility can be availed at the non-network hospitals. The hospital bills are directly settled at the hospital after the insured avails the treatment. The insured can then claim reimbursement for hospitalization by submitting relevant bills/documents for the claimed amount to IHA.
The insured can receive their claim after submitting necessary information and supporting documents in cash or by a bank transfer to the relevant accounts.
Complaints Management
Complaints officer from IHA and insurance body shall maintain complaints file. The file has the following:
- Unique registration number given to each complaint.
- Date of receipt of compliant
- Name & address of the complainant
- Date of acknowledging of the complaint.
- Details of action/ investigations.
- Date of closure
The complaints file is maintained by compliant officer. All correspondence in respect to complaints, investigation reports and decisions are filed in order. Based on the data gathered the compliant department will submit the result with insured. The insured also can directly contact via phone and share their compliant about any issue with IHA compliant department, IHA team will investigate the compliant and at the end the result will be communicating to the insured.